Food Allergy & Anaphylaxis
Anaphylaxis
If you or someone you know is experiencing an allergic reaction, please refer to your Allergy & Anaphylaxis Emergency Plan and call 911 immediately.
Anaphylaxis (an–a–fi–LAK–sis) is a serious allergic reaction that comes on quickly and has the potential to become life-threatening.
- Food, latex, insect stings and medicines can cause a severe allergic reaction(6).
- Anaphylaxis includes a wide range of signs and symptoms that can occur alone, or in combination, after exposure to an allergen.
- Symptoms can develop rapidly after exposure to an allergen, often within minutes and usually within 30 minutes. However, it can take up to 2 hours for symptoms to occur after exposure to a food allergen.
- Anaphylaxis requires immediate medical treatment, including an injection of epinephrine and a visit to the emergency room. Anaphylaxis can be fatal if not treated promptly.
- Observation in a hospital for a period between 4 and 24 hours is recommended once the individual has returned to normal, due to concerns of biphasic anaphylaxis.
- If you or someone you know is at risk of anaphylaxis, two epinephrine auto-injectable devices must be carried at all times.
Each year in the U.S., it is estimated that severe reactions to food cause:
- 30,000 emergency room visits
- 2,000 hospitalizations
- 150 deaths(5)
Biphasic Anaphylaxis is the recurrence of symptoms within 1-72 hours after initial symptoms have resided, typically occurring within >8 hours after the initial reaction. Approximately 20% of anaphylactic reactions recur within 4-6 hours. (7)
Biphasic reactions occur with no other exposure to an allergen and treated in the same manner as anaphylaxis. Biphasic incident reports vary, with some studies reporting occurrence in 25% of anaphylaxis cases, and may be more severe as the initial reaction.
Anaphylaxis: Signs and Symptoms Poster
Anaphylaxis FAACTs Poster
Allergy & Anaphylaxis Emergency Plan (AAP)
Anaphylaxis in the ED: A Reference for Physicians (ACAAI)
Epinephrine Auto-Injector Options
.jpg)
Anaphylaxis FAACT’s
- Food allergy is the leading cause of anaphylaxis.
- The sooner anaphylaxis is treated, the less severe it is likely to become.
- Delayed use of epinephrine has been associated with fatalities due to anaphylaxis.
- Anaphylaxis can occur without hives, and some studies show that fatalities are more common when there is anaphylaxis without hives.
- The severity of a reaction cannot be accurately predicted by the degree of severity of past reactions. An individual who previously had only “mild” reactions can later have dangerous and even life-threatening reactions. However, if an individual has a history of a severe reaction or anaphylaxis, then he/she is at high risk for having another severe reaction.
- In 70% of fatal or near fatal cases of food allergy reactions, there was either a delay in the administration of epinephrine, or epinephrine was not administered at all(8).
- Asthma, chronic lung disease, and cardiovascular disease increases risk of death from anaphylaxis.
- In one study, 25% of anaphylactic reactions at school involved individuals whose allergy was unknown at the time of the reaction.
- Epinephrine CAN be used to treat the symptoms of an anaphylactic reaction and an asthma attack. In fact, epinephrine was used to treat asthma attacks before other asthma medications were available. Asthma medication, however, will NOT treat an anaphylactic reaction. Speak to a board certified allergist for more information.
- All 50 states have laws allowing stock epinephrine. Only 11 states mandate schools to stock epinephrine, and the remainder states allow the option to stock this if they choose. There is a federal law that encourages states to pass laws allowing stock epinephrine.
- Visit FAACT's Education Resource Center for FREE and downloadable resources.
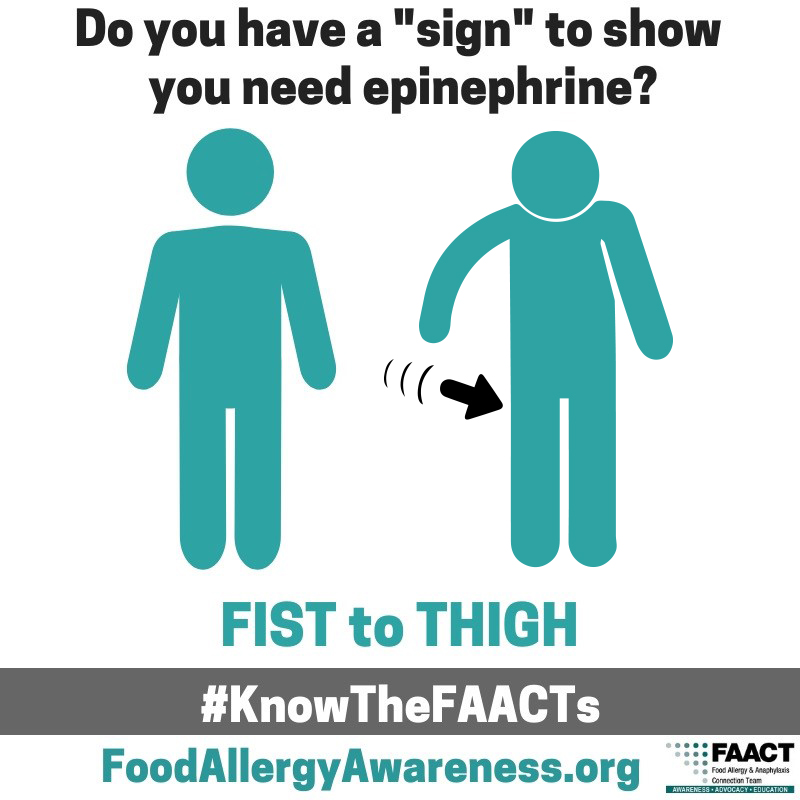
FAACT's FIST to THIGH "SIGN"
What would you do if you needed epinephrine...but you couldn't be heard?
Do you have a "SIGN"?
There might be a time when you are too far away for someone to hear you clearly or anaphylaxis is making it difficult to speak.
Here is a "SIGN" you can use...
- Move in motion
- FIST to THIGH
- Wait a second
- Repeat again
- FIST to THIGH
Download this "SIGN" and share with others so they can quickly respond in an emergency.
And, please share this video to help FAACT spread the word about this potentially life-saving "SIGN"!

More About Anaphylaxis
The most common anaphylactic reactions are to foods, venom from insect bites or stings, medications, and latex.
Anyone with a previous history of anaphylactic reactions is at risk for having another severe reaction. Also at risk are those with a personal or family history of allergic conditions (asthma, eczema, or allergic rhinitis). It is recommended to seek advice and treatment from a board-certified allergist, always carry two epinephrine auto-injectors (see graphic), and to obtain an Allergy & Anaphylaxis Emergency Plan.
Common associations with fatal food anaphylaxis are failure to administer epinephrine promptly, reactions involving peanuts and tree nuts, teenagers and young adults, patients with a history of food allergy and asthma, and individuals presenting respiratory symptoms.
Download FAACT's Poster for Epinephrine Auto-Injector Options.
Latex Allergy
Latex Allergy is allergy to natural rubber latex (Hevea brasiliensis). According to the Centers for Disease Control and Prevention, at least 7.7 million people are employed in the growing health care industry. While there are no overall statistics on the prevalence of latex allergy in that work force, studies do indicate that 8 to 12% of health care workers regularly exposed are sensitized, compared with 1 to 6% of the general population.
There are several Types of Latex Allergy; including Type IV Allergic Dermatitis, Type I IgE mediated allergy and Allergic Contact Dermatitis. Latex Allergic individuals can develop asthma or occupational asthma in addition to cross-reactive food allergies most commonly to banana, avocado, kiwi and chestnut
Symptoms can range from mild to severe, and can include one or more of the following:
• hives or welts
• swelling of affected area
• runny nose
• sneezing
• headache
• reddened, itchy or teary eyes
• sore throat, hoarse voice
• abdominal cramps
• chest tightness, wheezing, or shortness of breath (asthma)
If exposure to latex continues, allergy symptoms may include a severe and life-threatening allergic reaction called anaphylaxis.
The most common products containing natural rubber latex are latex gloves and balloons, but may be in many medical products and over 40,000 consumer products.
Diagnosis of latex allergy is most commonly done by medical history. Currently there is no cure for latex allergy. Individuals with latex allergy may have medications to reduce the symptoms and reactions of latex allergy. The only way to prevent an allergic reaction to latex is to avoid natural rubber latex products.
This Information was provided by the former American Latex Allergy Association (ALAA), now under the Allergy & Asthma Network.
For more information on Latex Allergy visit: http://www.allergyasthmanetwork.org/education/allergies/latex-allergy/
Airborne Exposure
Airborne reactions fortunately are not common.
There is no evidence that peanut or tree nut particles or dust become airborne and can be inhaled, triggering a reaction. One study has shown that peanut butter vapors cannot trigger a reaction (no protein content), and two studies have shown that peanut dust is undetectable in the air. What likely happens is that the dust rapidly settles and persons unknowingly get the particles on their hands, which then come into contact with mucus membranes (e.g., finger-to-mouth contamination). There have been substantiated reports of fish/shellfish vapor containing protein and triggering a reaction.
References:
1. Consortium for Food Allergy Research (CoFAR)
3. NIAID, Guidelines for the Diagnosis and Management of Food Allergy in the United States
5. FDA.gov. (2018). What You Need to Know about Food Allergies. [online] Available at: https://www.fda.gov/food/buy-store-serve-safe-food/what-you-need-know-about-food-allergies
6. CDC.gov. (2018). Food Allergies | Healthy Schools | CDC. [online] Available at: https://www.cdc.gov/healthyschools/foodallergies/index.htm
7. Biphasic systemic anaphylaxis: An inpatient and outpatient study. https://www.jacionline.org/article/S0091-6749(94)70044-3/fulltext