Education
For School Personnel
Back to Category View.jpg)
For School Personnel
With the increased number of students with food allergies now enrolled in schools – and 30 percent of food-allergic children allergic to multiple foods – increased education and resources for school personnel are essential.
True food allergies (as opposed to food intolerances) have the potential to become life-threatening. All school staff who interact with food-allergic students should understand the importance of food allergy management and the seriousness in food allergy reactions.
FAACT
Every food allergy reaction has the possibility of developing into a life-threatening and potentially fatal anaphylactic reaction.
.jpg)
Education for School Personnel
Educators are often the first to act in an emergency situation. Providing educators with the tools and information needed to care for food-allergic students will build the confidence needed to act quickly in an emergency.
Topics to cover in education for school personnel include basic food allergy medical facts, how to ensure students avoid allergens, the signs and symptoms of an allergic reaction, and how to enact emergency procedures. School policies and guidelines should include:
- Daily management of food allergies, allergen avoidance measures, emergency response, how to address bullying of and discrimination against students with food allergies.
- Strategic placement of medication, identifying the locations for school personnel and ensuring the medication is easily accessible and unlocked.
- Informing staff of all students who self-carry medications.
- Training school personnel in the administration of medications in accordance with governing laws.
- Working with the district’s transportation department on:
- Emergency procedures.
- “No food or beverage sharing” policies.
- Seat placement (while limiting potential for social isolation).
- Reporting harassment, bullying, or threats made against food-allergic students.
- Each student’s Allergy & Anaphylaxis Emergency Plan and other important information.
- Visit FAACT's Bus Drivers and Transportation Personnel section.
- Providing food allergy education for school personnel, students, parents, caretakers, and others who have contact with the student throughout the day.
- Identifying a core team to work with parents and the student to establish a prevention plan, including bus drivers, school counselors, teachers, substitute teachers, food service personnel, school administrators, the school nurse, and any other necessary individuals.
- Enforcing restrictions on permissible foods in the classroom and dedicated areas in the lunchroom.
- Arranging for emergency drills to include school personnel and first responders.
- Following applicable federal laws and identifying students with food allergies who qualify for Section 504 and other plans.
- State and federal laws that may apply to students with food allergies (e.g., stock epinephrine laws, self-carry medication laws).
- District policies and individual healthcare plans, 504 plans, etc., and procedures.
FAACT
Understanding how to enact emergency protocols in the event of an emergency ensures immediate action that could help save lives.
Download our free 'FAACTs for Schools' Staff Education Program.
The School’s Role
The school’s role in managing students with food allergies can seem daunting, especially for districts and schools currently that do not have a food allergy policy or guidelines in place.
At a minimum, FAACT recommends that schools require an Allergy & Anaphylaxis Emergency Plan (AAP) (signed by the student’s medical provider) for every food-allergic student and two auto-injectable epinephrine devices that are readily accessible, unlocked (or self-carried), and in a location known by every staff member in the school.
Each student’s emergency action care plan is like a guide on how to treat the student in the event of an emergency. It is signed by a doctor, giving the educator information on the student’s condition and specific instructions to follow should the signs and symptoms of an allergic reaction occur.
Partnering with parents and students will support efforts to improve the school setting for food-allergic students. Ask parents for guidance about the student – they are the experts on the child’s needs.
School staff should also carefully review the contents of this Web site and utilize the free downloads and resources available in FAACT's Education Resource Center to assist in caring for food-allergic students.
FAACTs
- In the school setting, when a school nurse or other licensed healthcare professional is not available to assist the student, the emergency action care plan should be as simple as possible.
- Allergy & Anaphylaxis Emergency Plan (AAP)
- A call to 9-1-1 and a trip to the emergency room should always follow epinephrine administration.
- Antihistamines alone should not be used to treat anaphylaxis. They can be administered after epinephrine. (See Treatment of Anaphylaxis for more details.)
- The signs and symptoms of an asthma attack and those of anaphylaxis can appear the same.Asthma medication (such as an albuterol inhaler) will only treat respiratory symptoms, while epinephrine will treat both an asthma symptoms and other symptoms of anaphylaxis.
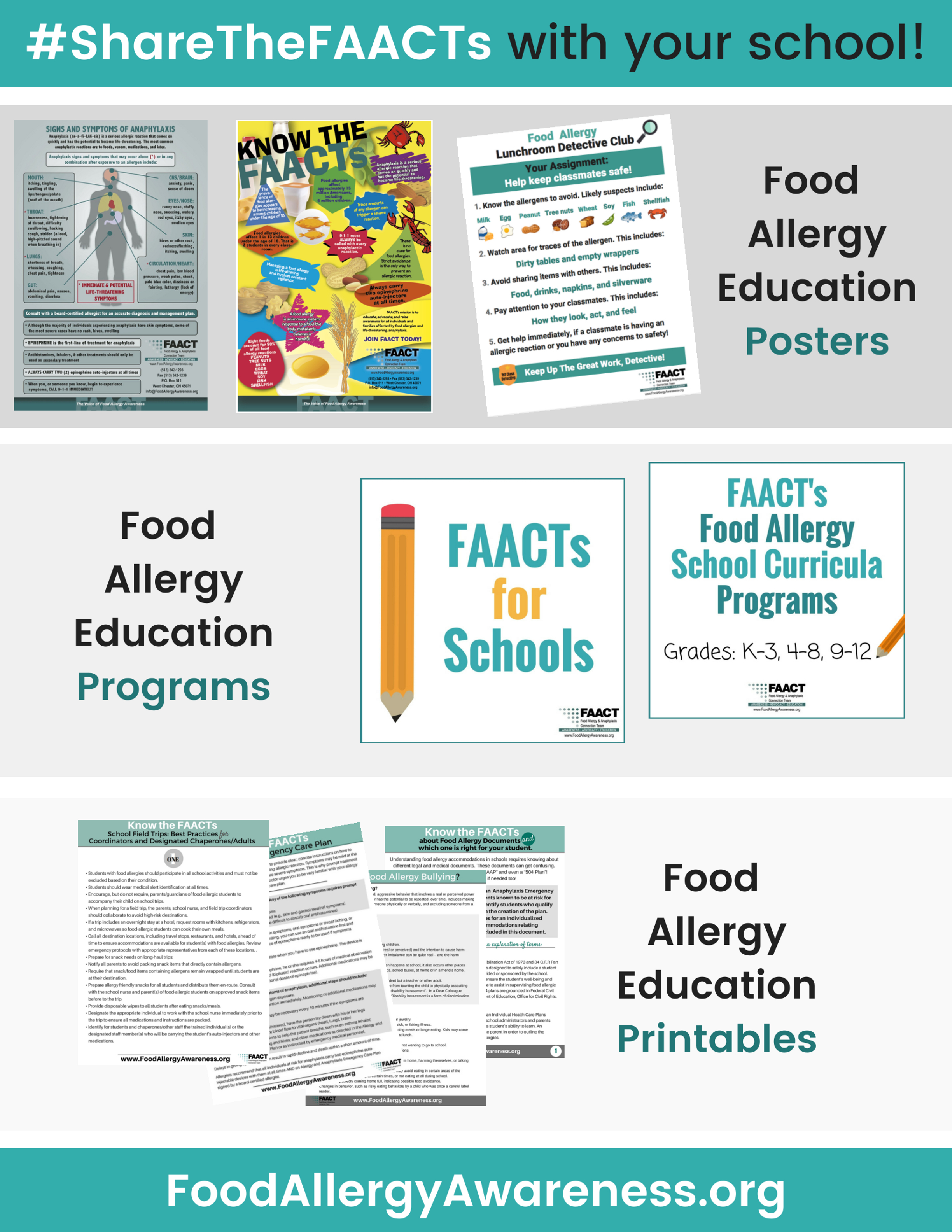
Resources for School Personnel
- FAACT's Food Allergy Curricula Program for Schools
- 'FAACTs for Schools' Program
- FAACT's School Lunchroom Poster
- FAACT's Food Allergy School Letter to Parents (Sample Template)
- CDC Voluntarily Guidelines or Managing Food Allergies in School
- Food Allergy Management & Education (FAME) Toolkit
- School Access to Emergency Epinephrine Act
- The Need for Stock Epinephrine Auto-Injectors and Comprehensive Food Allergy and Anaphylaxis Management Plans in Schools, an Article Review
School staff should carefully review the contents of this Web site and utilize the free downloads and resources available.
More information on food allergies in the school setting can be accessed in FAACT's Education Resource Center.
FAACT Posters
- 10 FAACTs about Food Allergies
- Allergy & Anaphylaxis Emergency Plan
- Anaphylaxis Locations in Schools
- Bullying - What Is Food Allergy Bullying?
- Bullying - Keys to Standing Up, Involvement, & Inclusion
- Bus Drivers & Transportation Personnel: Best Practices & Prepare to Act
- Bus Drivers & Transportation Personnel: Checklist
- Communicating with School Personnel: A Parents Guide
- FAACT's School Programs for School Personnel
- Field Trips - Best Practices
- Food Allergy Accommodations: Documents & Plans for School
- Food Allergy Education for School Personnel
- Food Allergy Safety - It's A Matter of FAACT!
- Food Service Personnel: Best Practices & Prepare to Act
- Newly Diagnosed with Food Allergies
- Preventing Cross-Contact
- Traveling with Food Allergies
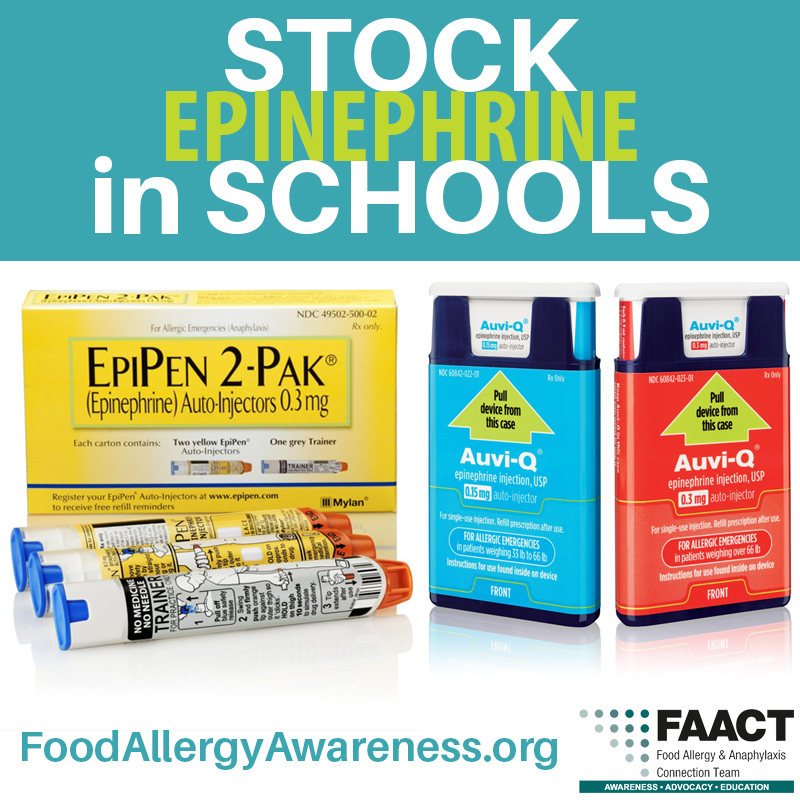
Stock Epinephrine in Schools
Many states have stock epinephrine laws in place that allow schools to keep a “stock” supply of epinephrine on schools grounds. Some laws allow for school staff trained in the administration of the medication to administer the medication to a student (and staff in some states) who appears to be in anaphylactic shock, whether the individual has a prescription or not.
In addition to protecting those who experience first-time anaphylaxis on school grounds, having the medication available also protects those who may require an additional dose of epinephrine or in case of a mechanical malfunction.
On November 13, 2013, President Obama signed into law the School Access to Emergency Epinephrine Act, which encourages states to adopt laws requiring schools to “stock” epinephrine auto-injectors. Financial incentives are provided for states mandating stock epinephrine in schools.
Learn more about stock epinephrine laws in your state by visiting the Government Relations section of FAACT’s website.
FAACTs
- 25 percent of first-time anaphylactic reactions reported in the school setting were those of students with no known history of an allergy.
- Studies report that 1 in 13 children in the United States have a food allergy. This averages to two children per classroom.
- In cases of fatalities from food allergy in the school setting, fatalities were associated with significant delays in administering epinephrine.
- 30 percent of children with food allergies are allergic to multiple foods.
- 1 out of 5 children with food allergies will have an allergic reaction while in school.
- Failure to properly recognize and a delay in treatment for anaphylaxis has led to fatalities in schools.
- Side effects of using epinephrine are usually mild and temporary
- In about one-third of anaphylactic reactions, a second round (or “phase”) of allergic reactions can occur after the initial anaphylactic reaction. This is called “biphasic anaphylaxis” A second reaction may happen as early as an hour after the first reaction or as long as 72 hours later (the average is 10 hours later) and can be less severe, as severe, or even more severe than the initial reaction.
- Every food allergy reaction has the possibility of developing into a life-threatening and potentially fatal reaction.
- There is no cure for food allergies. Avoidance is the only way to prevent a food allergy reaction from occurring.
- You cannot predict how severe a student’s reaction will be based on previous reactions. Students who previously had only “mild” reactions can later have dangerous and even life-threatening reactions.
- In approximately 20 percent of anaphylactic reactions, symptoms go away and will recur 1-3 hours later.
- More than 170 foods are known to cause a reaction in some people. However, eight foods account for 90 percent of all allergic reactions to foods:
- Milk
- Eggs
- Peanut
- Soy
- Wheat
- Tree nut (e.g., almonds, walnuts, pecans)
- Fish
- Shellfish (e.g., crab, lobster, shrimp)
References
6.↵ McIntyre CL, Sheetz AH, Carroll CR, Young MC. Administration of epinephrine for life-threatening allergic reactions in school settings. Pediatrics. 2005;116(5):1134–1140
5.↵ Sicherer SH, Furlong TJ, DeSimone J, Sampson HA. The US Peanut and Tree Nut Allergy Registry: characteristics of reactions in schools and day care. J Pediatr. 2001;138(4):560–565
10.↵ Sampson HA, Mendelson LM, Rosen JP. Fatal and near-fatal anaphylactic reactions to food in children and adolescents. N Engl J Med. 1992;327(6):380–384
11.↵ Bock SA, Muñoz-Furlong A, Sampson HA. Fatalities due to anaphylactic reactions to foods. J Allergy Clin Immunol. 2001;107(1):191–193
12. 2.↵ Bock SA, Muñoz-Furlong A, Sampson HA. Further fatalities caused by anaphylactic reactions to food, 2001–2006. J Allergy Clin Immunol. 2007;119(4):1016–1018
30.↵ Perry TT, Conover-Walker MK, Pomes A, Chapman MD, Wood RA. Distribution of peanut allergen in the environment. J Allergy Clin Immunol. 2004;113(5):973–976
2Management of food allergies in the school setting. Pediatrics. 2010; 126(6): 1232-1239. Sischer SH, Mahr T.